Nurses Have Had Enough, Threatening Big Gaps in US Health Care
 A large swath of American nurses want out of the profession, raising the threat of a mass exodus that would leave gaping holes in health care.
A large swath of American nurses want out of the profession, raising the threat of a mass exodus that would leave gaping holes in health care.
Almost one in three registered nurses say they’re likely to seek a different job, according to a recent survey by AMN Healthcare Services Inc. A McKinsey & Co. study last month warned the US risks a shortfall of as many as 450,000 nurses. Job openings in health care surged above 2 million in April, not far short of last year’s record.
The pandemic put nurses and other health-care professionals under unprecedented strain. The worst of the COVID crisis may be over, but staff remain stretched. And that’s creating a “vicious cycle” of fewer people wanting to become nurses as the profession becomes more stressful and less satisfying, according to Cole Edmonson, chief clinical officer at AMN.
“This really creates this negative narrative that can have implications for the workforce for years to come,” Edmonson says.
What’s more, just when the US urgently needs more nurses, enrollment in student programs fell for the first time in more than two decades last year. And the AMN survey found young nurses are significantly less satisfied with their careers than older colleagues – which bodes ill for the prospect of reversing that drop.
Employers have tried turning to foreign labor. Last fiscal year, the Commission on Graduates of Foreign Nursing Schools received over 17,000 applications to its visa screen program, which provides certification for foreign health-care professionals — more than twice the pre-pandemic number.
“The amount of work we’re doing for health-care institutions – we’ve always done some, it’s always been a big piece — but it’s taken off and exploded,” said Brendan Venter, an immigration lawyer at Harris Beach PLLC. Even employers who used to shy away from the bureaucracy and delays involved in bringing nurses from abroad are now “kind of forced into it,” he said.
‘Grow Our Own’
Even so, that’s a patch not a real fix. There’s strong political opposition to faster immigration. Plus, the supply of foreign nurses isn’t unlimited – and there’s a global bidding war under way, as many countries in similar straits to the US seek to recruit them.
“We’ll never make up for those shortages by bringing people in from abroad,” said Megan Cundari, senior director of federal relations at the American Hospital Association. “We need to grow our own nurses.”
Kathleen Polley-Payne, who’s executive director of the School of Nursing at the University of St. Augustine for Health Sciences in Florida, has some ideas how that could be done better. For one, the profession could use more gender diversity. “We need men coming into nursing,” she said. “Their perspective is different and fresh.”
For another, there needs to be a better path for people who want switch professions. “We’ve found a lot of people from finance and so forth were coming to nursing because they felt like they needed a purpose,” Polley-Payne said. A shorter qualification program for would-be nurses with degrees in something else would help, she says. So would measures that let employers make bigger contributions to help nurses repay student debt.
When there’s a shortfall of nurses, each of those who remain has to deal with more patients – exacerbating what’s already one of the job’s biggest downsides.
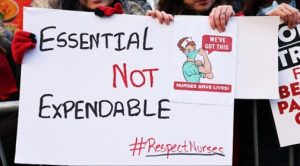
The pandemic has seen a series of strikes by nurses all over the country — the latest one began in Oregon last week, involving some 1,800 nurses and clinicians — and safe staffing levels, along with better compensation and benefits, have consistently featured among the demands.
‘Every Day Short’
Benny Mathew was a key voice in a three-day strike in January by 7,000 New York nurses, who sought to lock in higher staffing levels as well as better pay. “We are understaffed and we’re working every day short,” he said.
Mandating a minimum nurse-to-patient ratio is a widespread demand in the profession. Currently, only California has such rules, though it eased them in the COVID crisis. Democratic lawmakers introduced a bill this year to set similar criteria nationwide. It’s opposed by hospital groups, who say it would raise costs without necessarily improving care.
The McKinsey survey found that “not having a manageable workload” was one of the two main reasons cited by nurses planning to quit. (The other was “not feeling valued by their organization.)
On top of all the profession’s regular strains, former emergency-room nurse Hannah Berns said it was the pandemic that catalyzed her longstanding ambition to try something different. She’d been a registered nurse for a decade when COVID-19 arrived, but “being so vulnerable in a work environment was scary.”
Now she’s swapped her ER job in San Francisco for a “quote-unquote normal life” working at a digital publication for nurses, after getting her master’s during the pandemic. “I absolutely miss the hospital setting,” she says. “But at the same time, the burnout that was associated with it, the long shifts, the violence — it’s unacceptable.”
(This story originally appeared in the Union-Democrat via Bloomberg News.)
/”_blank” bg_color=”#d2232a” btn_hover_bg=”#211f5d”]Read More[/mk_button]



